THE USE OF DIGITAL DEVICES IN THE STUDY INCREASES MIGRAINE INCIDENCE AMONG MEDICAL STUDENTS, KAU, SAUDI ARABIA
Aysha A. ALSHRAEEF 1*, Omar M. ALHAZMI 2
1 Internal Medicine Department, Neurology Unit, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia.
2 Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia.
*Corresponding Author
ABSTRACT
Migraine is the most popular neurological condition which affects virtually everybody during their lifetime minimally once. Globally, migraine has a high prevalence among medical college students. This research aimed to determine whether there is an association between learning from electronic devices and migraine prevalence between medical students at King Abdulaziz University (KAU), Jeddah, Saudi Arabia. This cross-sectional study was carried out on 398 students (both sexes) in different academic years at the faculty of medicine, KAU, Jeddah, Saudi Arabia. The data were collected using a closed-ended questionnaire. The results revealed that more than half of the participants (52.5%) suffered from migraine in earlier periods of their lives. The key indicators of migraine were female (60.8%), school days (90.9%), positive family history (76.6%), adolescence (54.1%), an electronic source in studying (52.2%), and screen exposure for more than 4 hours daily (61.3%). Furthermore, there was a significant association between migraine and gender, family history, electronic source of study, duration of screen exposure, and adolescence. The findings of this research revealed that students of the medical school who suffer from migraine could be attributed to the usage of digital study methods such as a laptop, a computer, or a tablet in studying with screens exposure for long periods.
Keywords: Migraine, medical students, digital devices, screens exposure, gender, family history
INTRODUCTION
Migraine is the most common neurological disorder (Mosarrezaii and Kargar, 2018; Ramadan et al., 2019; Alshammari et al., 2019). It is a chronic and sometimes progressive multifactorial neurological disorder. It is commonly prevalent in young adults, especially females by the onset of puberty; they comprise two-third of this disorder due to the hormonal changes; also, it is more prevalent in people with high educational levels (Wahab and Ugheoke, 2009; Balaban et al., 2012). The prevalence of migraine peaks during the most productive years of adulthood (age 25 to 55 years) (Lipton and Bigal, 2005).
Migraine is a significant health problem that has essential impacts on patients' daily activities and the quality of life (Domingues et al., 2009; Houinato et al., 2010). It is characterized by pulsatile episodes of headache, unilateral, which remain from 4 to 72 hours (Lusić, 2001; Bigal et al., 2006). Vomiting, nausea, photophobia, disability, and loss of performance are commonly accompanying migraine (Lampl et al., 2003; Houinato et al., 2010; Neut et al., 2012; Vuković et al., 2010). The most common trigger factors of migraine are stress, sleep disorders, fever, anxiety, poor eating habits, food items, changes in weather conditions, poor physical activities, menstrual cycle, oral contraceptives, and smoking (Vlajinac et al., 2003; Bessisso et al., 2005; Ertas et al., 2012).
Recently, the use of electronic devices as smartphones, computers, tablets is increased in academic study, especially among young people. High education students are heavily exposed to screens because of the increasing use of technology devices for their academic work (Fountaine et al., 2011). Previous researches showed a positive association between screen time exposure and migraine (Kurt and Kaplan, 2008; Smitherman et al., 2011). Similarly, the use of electronic devices was associated with migraine (Torsheim et al., 2010).
Numerous previous studies showed that students, especially those who are experiencing high levels of stress, are more susceptible to severe episodes of migraine (Radtke and Neuhauser, 2009; Yazdanparast et al., 2013). Al-Hashel and his colleges found that migraine is more prevalence among medical students in Kuwait University compared to other students. In addition, they reported that the severity and frequency of the migraine increase in the final two years. Their results also showed that the most common trigger factors of migraine are stress, increase in reading hours, especially from electronic devices, and irregular sleep (Al-Hashel et al., 2014).
Globally, migraine prevalence among medical students ranges from 11 to 40 % (Galinović et al., 2009; Ferri-de-Barros et al., 2011). It harms university students; they have limited daily activities, low concentrations, and impaired academic performance and success. This may influence their future occupational performance in society (Amayo et al., 2002; Smitherman et al., 2011; Balaban et al., 2012).
There are few studies done on migraines among medical students in Jeddah, Saudi Arabia. Medical students are the most subjected students to stress and responsibility during their academic years. They are also exposed to electronic screens for a long hour at the university (as teaching aids) and throughout the day (as studying aids).
This study aimed at investigating if there is an association between studying from electronic sources and migraine prevalence in medical students at KAU, Jeddah, Saudi Arabia.
SUBJECTS AND METHODS
Study design
This cross-sectional study was carried out at the faculty of medicine, KAU hospital, Jeddah, Saudi Arabia. It was conducted over six months in the academic year 2018-2019. The participants were selected based on the inclusion and exclusion criteria. The study was approved by the Unit of Biomedical Ethics, Research Ethics Committee, Faculty of Medicine, KAU, Saudi Arabia.
Determination of sample size
Estimated population of the medical students at KAU, Jeddah in 2018-2019 academic year is 2500 (population size=2500), the confidence level (z)=1.96, the margin of error (e)=0.05, sample proportion of uncertain = 0.05; therefore the sample size should be up to 343 students.
Inclusion criteria
Medical students of various medical fields at KAU in all academic years.
Exclusion criteria
Non-medical student at KAU.
Study sampling
This study conducted with 398 students in different academic years from both sexes. All the participants included in this study were asked to sign a written consent form.
Data collection
The data were collected using a closed-ended questionnaire. The following information was collected including gender, academic year, presence of migraine, having a family history of migraine, the duration time from headache problem start, duration of use tablets or computers for daily study, the source used for the daily study, number of headaches occurs, headache associated symptoms, and risk factors of headaches. For content validity, the questionnaire was initially translated into Arabic, after being modified according to the pre-tested for question accuracy and clarity then converted back to English. To protect the privacy of participants, no personal documentation details were collected, and anonymous and voluntary participation was ensured.
Statistical analysis
All statistical analyses were performed using GraphPad Prism software version 5. Data were presented as frequencies and percent for quantitative data, and the Chi-Square test for association (p < 0.05 was statistically significant).
RESULTS
In this study, the total number of participants was 398 students. 188 students were male (47.2%), and 210 were female (52.8%). The participants were distributed between the different academic years as follows: the second academic year (84, 21.1%), resident doctor (67, 16.8%), the sixth academic year (65, 16.3%), the fifth academic year (48, 12.1%), the third academic year (47, 11.8%), intern doctor (44, 11.1%), and the fourth academic year (43, 10.8%). More than half of the participants (209, 52.5%) suffered from migraines in earlier periods of their lives, while the rest (189, 47.5%) were told they had not had migraines previously (Table 1).
Table 1: Characteristics of the participants according to gender, academic year and history of migraine attacks.
|
|
Frequency (n) |
Percent of total (%) |
|
Gender |
||
|
Male |
188 |
47.2 |
|
Female |
210 |
52.8 |
|
Academic year |
||
|
Second |
84 |
21.1 |
|
Third |
47 |
11.8 |
|
Fourth |
43 |
10.8 |
|
Fifth |
48 |
12.1 |
|
Sixth |
65 |
16.3 |
|
Intern doctor |
44 |
11.1 |
|
Resident doctor |
67 |
16.8 |
|
Have you had a migraine beforehand? |
||
|
Yes |
209 |
52.5 |
|
No |
189 |
47.5 |
Total n=398 students. Data presented as number (n) and percent of total (%).
The total number of the participants having migraines was 209, among them 82 (39.2 %) were male and 127 (60.8%) were female. This indicated that migraine is more prevalent in female than in the male. The headache problems of most of the participants (88; 42.1%) started more than five years ago. It was found that 64 (30.6%) participants had headaches since 2-5 years ago, 34 (16.3%) participants since 1-2 years ago, and 23 participants since 6-12 months ago. The majority of the participants (190; 90.9%) said that the headache increase during school days, while only (19; 9.1%) of them reported that the headache increase during the weekend. Most of the participants (160; 76.6%) had a family history of migraine, while 49 (23.4%) had no family history of migraine. More than half of the study participants (113; 54.1%) suffered from the headache at adolescence, 82 (39.2%) suffered from the headache at 20-25 years, and only 14 (6.7%) suffered from the headache at childhood (Table 2).
Concerning the sources used for the daily study, the majority of the participants either used electronic sources only or electronic (109; 52.2%) and books (86; 41.1%), while 14 (6.7%) used the books only for the daily study. Regarding the duration of use of tablets or computers for daily study, most of the participants (128; 61.3%) used electronic devices more than 4 hours, 41 (19.6 %) for 3-4 hours, 22 (10.5%) for 2-3 hours, and 18 (8.6%) for 1-2 hours (Table 2).
Table 2: Prevalence of migraine according to the students’ gender, the onset of headache, the period of headache, the family history, the duration and sources used for daily study, number of headaches occur/week and/or month, headache-associated symptoms, and risk factors of headaches.
|
|
Frequency (n) |
Total migraine cases (%) |
|
Gender |
||
|
Male |
82 |
39.2 |
|
Female |
127 |
60.8 |
|
When did your headache problem start? |
||
|
6-12 months |
23 |
11 |
|
1-2 year |
34 |
16.3 |
|
2-5 year |
64 |
30.6 |
|
> 5 years |
88 |
42.1 |
|
The headache increases during |
||
|
School days |
190 |
90.9 |
|
Weekend |
19 |
9.1 |
|
Does any member of the family has a migraine? |
||
|
Yes |
160 |
76.6 |
|
No |
49 |
23.4 |
|
Duration of use of tablets or computers for daily study |
||
|
1-2 hour |
18 |
8.6 |
|
2-3 hours |
22 |
10.5 |
|
3-4 hours |
41 |
19.6 |
|
> 4 hours |
128 |
61.3 |
|
The source used for the daily study |
||
|
Books |
14 |
6.7 |
|
Electronic |
109 |
52.2 |
|
Both |
86 |
41.1 |
|
Did you suffer from a headache at a previous age? |
||
|
Childhood |
14 |
6.7 |
|
Adolescence |
113 |
54.1 |
|
20-25 years |
82 |
39.2 |
|
The number of times headaches occur |
||
|
Daily |
11 |
5.3 |
|
< 3 times weekly |
64 |
30.6 |
|
> 3 times weekly |
64 |
30.6 |
|
< 10 times monthly |
70 |
33.5 |
|
Is headache accompanied by nausea? |
||
|
Yes |
176 |
84.2 |
|
No |
33 |
15.8 |
|
Severe headache with sensitivity to light or sound |
||
|
Yes |
198 |
94.7 |
|
No |
11 |
5.3 |
|
Vision disturbances that lasted from 5 to 60 minutes, followed by severe headache |
||
|
Yes |
166 |
79.4 |
|
No |
43 |
20.6 |
|
Does any of the options mentioned cause your headache? |
||
|
Lack of sleep |
109 |
52.2 |
|
Too much caffeine |
17 |
8.1 |
|
When exposed to stress and exam days |
83 |
39.7 |
Total n=398 students. Data presented as number (n) and percent of total (%).
About the number of headaches occurrence, most of the participants (70; 33.5%) suffered from migraine less than 10 times/month, 64 (30.6%) more than 3 times/week, 64 (30.6%) less than 3 times/week, and 11 (5.3%) suffered from daily attacks. Regarding headache-associated symptoms, 176 (84.2%) of the participants had migraine accompanied by nausea, 198 (94.7%) of the participants had migraine accompanied by sensitivity to light or sound, and 166 (79.4%) of the participants had migraine accompanied by vision disturbances lasted from 5 to 60 minutes. Regarding the factors that precipitated the migraine attacks, more than half of the participants (109; 52.2 %) reported that “the lack of sleep caused headache”, 83 (39.7%) of them reported “the exposure to stress and exam days caused the headache”. Only 17 (8.1%) of the participants mentioned that “too much caffeine caused headache” (Table 2).
The test of the association between gender and migraine showed that there was a significant association (p=0.0008) between migraine and gender. Migraine was more prevalent among females compared to males; 82 males had a migraine and 106 did not have a migraine, while 127 females had a migraine and 83 did not have migraine (Figure 1).
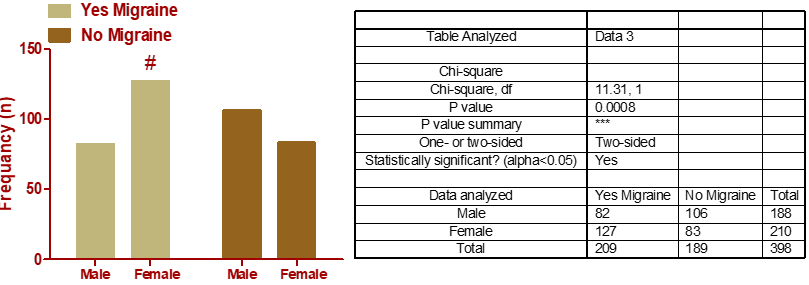
Figure 1: The association between gender and migraine. Total n=398 students. # Significant association between the migraine and the gender.
Concerning the association between migraine occurrence and the family migraine history, the data showed that there was a significant association (p < 0.0001) between migraine and the migraine history in the participant's family members. Migraine was more prevalent among participants with a positive family history of migraine compared to participants with a negative family history of migraine. One hundred sixty participants who suffered from migraines showed that also their family members suffered from migraines. 125 of the participants who did not suffer from migraines showed that also their family members did not suffer from migraine, and this could be an indicator that migraine is associated with a heredity factor (Figure 2).
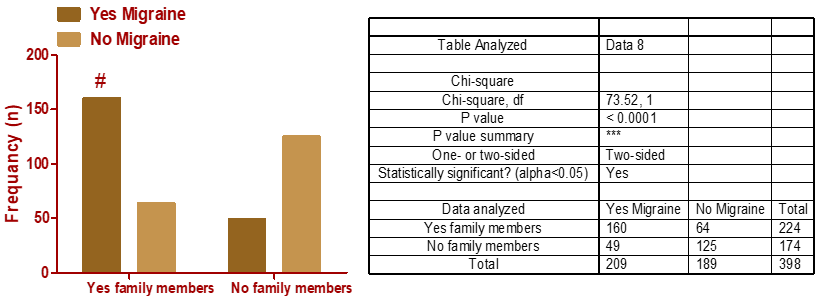
Figure 2: The association between a positive family history of migraine and migraine occurrence. Total n=398 students. # Significant association between the migraine and the family migraine history.
Concerning the association between the source used for the daily study and migraine, the obtained results revealed that there was a significant association (p < 0.0001) between the source used for the daily study and migraine. Migraine was more prevalent in the participants who used electronic devices daily, followed by those who used both electronic and books, and the least in the participants who used only books for the daily study. This indicates that using electronic devices increases the incidence of migraine (Figure 3).
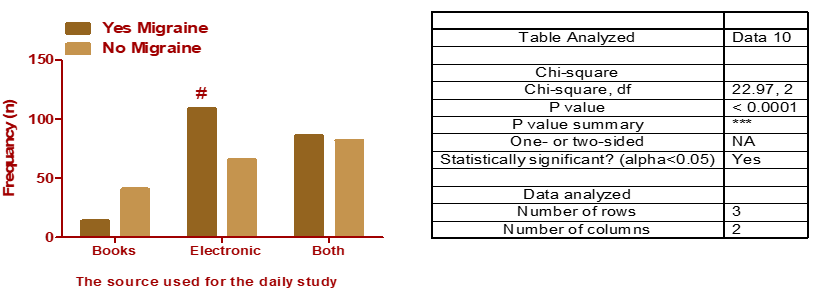
Figure 3: The association between the source used for the daily study and migraine. Total n=398 students. # Significant association between the migraine and the source used for the daily study.
Regarding the association between duration of use of tablets or computers for daily study and migraine, the obtained results showed that there was a significant association (p < 0.0186) between them. Participants who used electronic devices daily for more than 4 hours had migraine more than participants who used electronic devices daily for 1-2 hours. This suggested that when the duration of using electronic devices increase, the incidence of migraine increase (Figure 4).
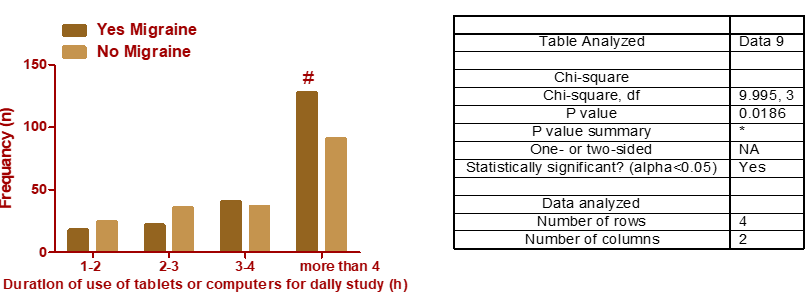 Figure 4: The association between duration of use of tablets or computers for daily study and migraine. Total n=398 students. # Significant association between the migraine and the duration of use of electronic devices daily.
Figure 4: The association between duration of use of tablets or computers for daily study and migraine. Total n=398 students. # Significant association between the migraine and the duration of use of electronic devices daily.
Concerning the association between the history of headache and the development of migraine, the data showed that there was a significant association (p= 0.0006) between migraine and participants having a history of headache at past age. Migraine was more prevalent among participants having a history of headaches at adolescence, followed by 20-25 years. These results revealed that the previous history of a headache increases the incidence of migraine (Figure 5).
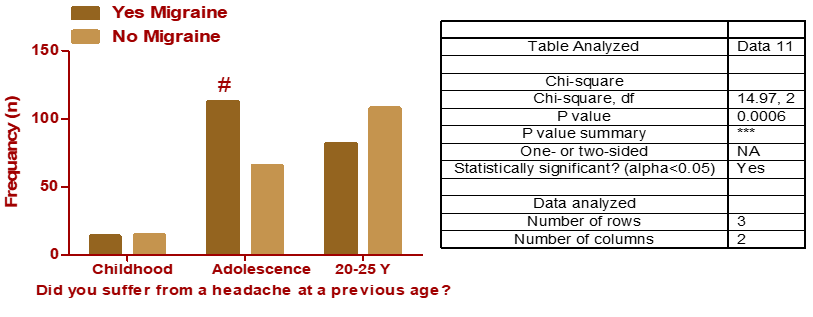
Figure 5: The association between the history of headache and migraine. Total n=398 students. # Significant association between the migraine and the history of headache.
DISCUSSION
The results of this study showed that more than half (52.5%) of the participants suffered from migraines in previous periods. In addition, our results showed that 79.4% of our migraine-experienced participants suffered from vision disturbances that lasted from 5 to 60 minutes before severe migraine attacks (migraine with aura). It emerged from this study that migraine occurs at a higher rate in the adolescent group by 54.1%, which showed a statistically significant difference when compared to the group without migraine. The migraine in students had less than 10 incidents a month. The study also showed that there is an association between the migraine and the gender of the participant, as it appears at a high rate in females (62.8%) compared to males (39.2%) (p < 0.001).
Several previous epidemiological studies of migraine have identified marked gender variation, as migraine has been particularly prevalent in females (Weitzel et al., 2001; Warhurst et al., 2018; Guo et al., 2019). Several theories have been suggested to clarify these variations in migraine, such as sex hormone, receptor binding, hereditary causes, discrepancies in the sensitivity to environmental triggers, and also some variations in responsiveness to stress (Fillingim et al., 2005; Gasbarri et al., 2008; Wang et al., 2008; Liverman et al., 2009; Martin, 2009). One of the explanations for this may be the effect of estrogen, which allows menstrual migraine attacks to occur without an aura and has increased length, weakness, and rigidity to therapy (Brandes, 2006).
The results of this research also showed that participants with migraine reported a migraine history in their family, as the study found a statistically significant difference between patients with migraine who had a family history of migraine compared to non-patients (p<0.0001). Family history has been recognized for a long time as a clinical diagnostic factor for migraine (Ducros et al., 2002). Family and twin research also shows that typical migraine is a hereditary disease, with an average heritage prevalence ranging among 30 and 60% (Mulder et al., 2003; Polderman et al., 2015; Sutherland et al., 2019). It has a clear genetic origin revealed by unique migraine conditions triggered by mutations in single genes (monogenic), and perhaps the popular familial aggregation of migraine correlated with polymorphisms in multiple genes (polygenic) (Sutherland and Griffiths, 2017).
The results of this study also revealed that migraine increases during the school days, as 90.9 % of the participants were told. On the other hand, only 9.1 % of the participants were suffering from headache at the weekends. Furthermore, the results of this study showed that lack of sleep is one of the most significant (52.2%) triggers of migraine in medical school students, followed by exposure to stress during exams periods (39.7%), while caffeine consumption came in the last place (8.1%) as a factor accompanying the occurrence of migraine. The most popular causes of migraine in previous research were tension at work or study (91.25%) and poor sleep (90%) (Gu and Xie, 2018). In addition, a variety of study findings reported that the two leading causes of migraine assaults in medical graduates are tension and sleep disturbance (Shahrakai et al., 2011; Ezeala-Adikai et al., 2013; Al-Hashel et al., 2014; Noor et al., 2016). Hence, stress reduction approaches will be designed to allow the students to know the correct stress control methods (Gu and Xie, 2018).
The main objective of this study was to find out whether there is an association between the use of electronic study resources (laptop, tablet, and desktop computer) in studying and the higher percentage of migraine attacks among medical school students compared to using books and publications. The results of this study found an association between the use of electronic learning resources in studying and the occurrence of migraine, as the number of users of electronic sources increased in students who were exposed to migraine attacks compared to non-migraine participants (p<0.0001). On the other hand, the percentage of students suffering from migraine who rely on electronic learning sources has reached 52.2%, and second came students using a mix of learning sources (electronic and books) (41.1%), while the last ranked percentage was students depending on studying on books and publications (6.7%). Many patients with migraines are not only particularly susceptible to visual stimulation after episodes, as this may cause anew episode (Shepherd, 2010), but also, they are often prone during episodes (Martín et al., 2011). In migraine, visual provokers are essential since they are simple to control. It is recommended that the evaluation of patients with migraine by health care providers will involve concerns about visible causes and visual tension (Harle et al., 2006).
The results of the current research also showed that exposure to computer and tablet screens for more than 4 hours a day was accompanied by an increase in the incidence of migraine (61.3%), which showed a significant difference compared to those without migraine. As mentioned in a previous study on a large sample of health research students who study through the internet, there is a direct association between the number of hours of exposure to computer screens and the occurrence of a migraine (Montagni et al., 2016). Our results are compatible with preceding studies in a population of children and teens, which identified an association between screen time use and migraine in people who use electronic devices daily (Rossi et al., 2008; Iannotti et al., 2009; Taehtinen et al., 2014). A few reports measured the incidence of migraine among university students and medical students according to the computer time exposure (Deleu et al., 2001; Smitherman et al., 2011; Ghorbani et al., 2013). The proposed theory to understand whether screen time may interfere with the pathophysiology of migraine proposed that radiance or brightness of screen band light will have a migraine trigger effect (Deleu et al., 2001; Montagni et al., 2016).
CONCLUSION
The results of this research showed that medical students suffering from migraines could be due to the usage of electronic devices such as a desktop computer, a laptop, or a tablet in their study and long-term exposure to their screen.
Conflict of interest
There is no conflict of interest hindering this study.
Financial resources
There is no financial resources obstacle the study.
Study limitations
The number of cases participating in the study is limited, as a large number of them appeared without migraines.
References
Al-Hashel, J. Y., Ahmed, S. F., Alroughani, R., & Goadsby, P. J. (2014). Migraine among medical students in Kuwait University. The journal of headache and pain, 15(1), 26, 1-6. https://doi.org/10.1186/1129-2377-15-26.
Alshammari, Y. H. M., Aldoghmi, A. K. B., AlAfif, H. S. A., Alfayi, B. A., Alrebh, A. H., Alsayafi, Z. A., Fatani, Y. A., Aldughmi, A. N., Alzaidan, A. M., Alsubaiei, S. A. O. & Alqethami, S. S. (2019). Multiple Sclerosis Diagnosis and Management: A simple Literature Review. Archives of Pharmacy Practice, 10(4), 33-37.
Amayo, E. O., Jowi, J. O., & Njeru, E. K. (2002). Headache associated disability in medical students at the Kenyatta National Hospital, Nairobi. East African medical journal, 79(10), 519-523. https://doi.org/10.4314/eamj.v79i10.8813.
Balaban, H., Semiz, M., Şentürk, İ. A., Kavakçı, Ö., Cınar, Z., Dikici, A., & Topaktaş, S. (2012). Migraine prevalence, alexithymia, and post-traumatic stress disorder among medical students in Turkey. The journal of headache and pain, 13(6), 459-467.
Bessisso, M. S., Bener, A., Elsaid, M. F., Al-Khalaf, F. A., & Huzaima, K. A. (2005). Pattern of headache in school children in the State of Qatar. Saudi medical journal, 26(4), 566-570.
Bigal, M. E., Liberman, J. N., & Lipton, R. B. (2006). Age-dependent prevalence and clinical features of migraine. Neurology, 67(2), 246-251. https://doi.org/10.1212/01.wnl.0000225186.76323.69.
Brandes, J. L. (2006). The influence of estrogen on migraine: a systematic review. Jama, 295(15), 1824-1830. https://doi.org/10.1001/jama.295.15.1824.
Deleu, D., Khan, M. A., Humaidan, H., Al Mantheri, Z., & Al Hashami, S. (2001). Prevalence and clinical characteristics of headache in medical students in Oman. Headache: The Journal of Head and Face Pain, 41(8), 798-804. https://doi.org/10.1046/j.1526-4610.2001.01146.x.
Domingues, R. B., Cezar, P. B., Schmidt Filho, J., Moraes Filho, M. N. D., Pinheiro, M. N., Marchiori, J. G., ... & Domingues, S. A. (2009). Prevalence and impact of headache and migraine among Brazilian Tupiniquim natives. Arquivos de neuro-psiquiatria, 67(2B), 413-415. https://doi.org/10.1590/S0004-282X2009000300008.
Ducros, A., Tournier-Lasserve, E., & Bousser, M. G. (2002). The genetics of migraine. The Lancet Neurology, 1(5), 285-293. https://doi.org/10.1016/S1474-4422(02)00134-5.
Ertas, M., Baykan, B., Orhan, E. K., Zarifoglu, M., Karli, N., Saip, S., ... & Siva, A. (2012). One-year prevalence and the impact of migraine and tension-type headache in Turkey: a nationwide home-based study in adults. The journal of headache and pain, 13(2), 147. https://doi.org/10.1007/s10194-011-0414-5.
Ezeala-Adikai, B. A., Ekenze, O. S., & Onwuekwe, I. O. (2013). Frequency and pattern of migraine among medical and nursing students at Enugu, South East Nigeria. The journal of headache and pain, 14(1), 1-1. https://doi.org/10.1186/1129-2377-14-s1-p5.
Ferri-de-Barros, J. E., Alencar, M. J. D., Berchielli, L. F., & Castelhano Junior, L. C. (2011). Headache among medical and psychology students. Arquivos de neuro-psiquiatria, 69(3), 502-508. https://doi.org/10.1590/s0004-282x2011000400018.
Fillingim, R. B., Hastie, B. A., Ness, T. J., Glover, T. L., Campbell, C. M., & Staud, R. (2005). Sex-related psychological predictors of baseline pain perception and analgesic responses to pentazocine. Biological psychology, 69(1), 97-112. https://doi.org/10.1016/j.biopsycho.2004.11.008.
Fountaine, C. J., Liguori, G. A., Mozumdar, A., & Schuna Jr, J. M. (2011). Physical activity and screen time sedentary behaviors in college students. International Journal of Exercise Science, 4(2), 3.
Galinović, I., Vuković, V., Trošelj, M., Antić, S., & Demarin, V. (2009). Migraine and tension-type headache in medical students: a questionnaire study. Collegium antropologicum, 33(1), 169-173.
Gasbarri, A., Arnone, B., Pompili, A., Cifariello, A., Marini, C., Tavares, M. C., & Tomaz, C. (2008). Emotional memory and migraine: Effects of amitriptyline and sex related difference. Behavioural brain research, 189(1), 220-225. https://doi.org/10.1016/j.bbr.2007.12.009.
Ghorbani, A., Abtahi, S. M., Fereidan-Esfahani, M., Abtahi, S. H., Shemshaki, H., Akbari, M., & Mehrabi-Koushki, A. (2013). Prevalence and clinical characteristics of headache among medical students, Isfahan, Iran. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, 18(Suppl 1), S24.
Gu, X., & Xie, Y. (2018). Migraine attacks among medical students in Soochow University, Southeast China: a cross-sectional study. Journal of pain research, 11, 771. https://doi.org/10.2147/JPR.S156227.
Guo, Y., Xu, S., Nie, S., Han, M., Zhang, Y., Chen, J., ... & Liu, X. (2019). Female versus male migraine: an event-related potential study of visual neurocognitive processing. The journal of headache and pain, 20(1), 38. https://doi.org/10.1186/s10194-019-0995-y.
Harle, D. E., Shepherd, A. J., & Evans, B. J. (2006). Visual stimuli are common triggers of migraine and are associated with pattern glare. Headache: The Journal of Head and Face Pain, 46(9), 1431-1440. https://doi.org/10.1111/j.1526-4610.2006.00585.x.
Houinato, D., Adoukonou, T., Ntsiba, F., Adjien, C., Avode, D. G., & Preux, P. M. (2010). Prevalence of migraine in a rural community in south Benin. Cephalalgia, 30(1), 62-67. https://doi.org/10.1111/j.1468-2982.2009.01894.x.
Iannotti, R. J., Kogan, M. D., Janssen, I., & Boyce, W. F. (2009). Patterns of adolescent physical activity, screen-based media use, and positive and negative health indicators in the US and Canada. Journal of Adolescent Health, 44(5), 493-499. https://doi.org/10.1016/j.jadohealth.2008.10.142.
Kurt, S., & Kaplan, Y. (2008). Epidemiological and clinical characteristics of headache in university students. Clinical neurology and neurosurgery, 110(1), 46-50. https://doi.org/10.1016/j.clineuro.2007.09.001.
Lampl, C., Buzath, A., Baumhackl, U., & Klingler, D. (2003). One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia, 23(4), 280-286. https://doi.org/10.1046/j.1468-2982.2003.00509.x.
Lipton, R. B., & Bigal, M. E. (2005). Migraine: epidemiology, impact, and risk factors for progression. Headache: The Journal of Head and Face Pain, 45, S3-S13. https://doi.org/10.1111/j.1526-4610.2005.4501001.x.
Liverman, C. S., Brown, J. W., Sandhir, R., McCarson, K. E., & Berman, N. E. (2009). Role of the oestrogen receptors GPR30 and ERα in peripheral sensitization: relevance to trigeminal pain disorders in women. Cephalalgia, 29(7), 729-741. https://doi.org/10.1111/j.1468-2982.2008.01789.x.
Lušić, I. (2001). Population variation in migraine prevalence–the unsolved problem. Collegium antropologicum, 25(2), 695-701.
Martín, H., Del Río, M. S., De Silanes, C. L., Álvarez‐Linera, J., Hernández, J. A., & Pareja, J. A. (2011). Photoreactivity of the occipital cortex measured by functional magnetic resonance imaging–blood oxygenation level dependent in migraine patients and healthy volunteers: pathophysiological implications. Headache: The Journal of Head and Face Pain, 51(10), 1520-1528. https://doi.org/10.1111/j.1526-4610.2011.02013.x.
Martin, V. T. (2009). Ovarian hormones and pain response: a review of clinical and basic science studies. Gender medicine, 6, 168-192. https://doi.org/10.1016/j.genm.2009.03.006.
Montagni, I., Guichard, E., Carpenet, C., Tzourio, C., & Kurth, T. (2016). Screen time exposure and reporting of headaches in young adults: A cross-sectional study. Cephalalgia, 36(11), 1020-1027. https://doi.org/10.1177/0333102415620286.
Mosarrezaii, A., & Kargar, K. (2018). Frequency of Depression in Patients with Seizure Referring to the Urmia Neuromedical Clinic and Some of the Factors Affecting it. Journal of Advanced Pharmacy Education & Research| Apr-Jun, 8, 2.
Mulder, E. J., Van Baal, C., Gaist, D., Kallela, M., Kaprio, J., Svensson, D. A., ... & Boomsma, D. I. (2003). Genetic and environmental influences on migraine: a twin study across six countries. Twin Research and Human Genetics, 6(5), 422-431. https://doi.org/10.1375/136905203770326420.
Neut, D., Fily, A., Cuvellier, J. C., & Vallée, L. (2012). The prevalence of triggers in paediatric migraine: a questionnaire study in 102 children and adolescents. The journal of headache and pain, 13(1), 61-65. https://doi.org/10.1007/s10194-011-0397-2.
Noor, T., Sajjad, A., & Asma, A. (2016). Frequency, character and predisposing factor of headache among students of medical college of Karachi. J Pak Med Assoc, 66(2), 159-164.
Polderman, T. J., Benyamin, B., De Leeuw, C. A., Sullivan, P. F., Van Bochoven, A., Visscher, P. M., & Posthuma, D. (2015). Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nature genetics, 47(7), 702. https://doi.org/10.1038/ng.3285.
Radtke, A., & Neuhauser, H. (2009). Prevalence and burden of headache and migraine in Germany. Headache: The Journal of Head and Face Pain, 49(1), 79-89. https://doi.org/10.1111/j.1526-4610.2008.01263.x.
Ramadan, M., Mohammad, B., Karim Hussein, A. N., & Ahmed, A. (2019). The effect of long term treatment with betablockers in increasing the incidence of bradycardia in patients undergoing posterior segment eye surgeries. Journal of Advanced Pharmacy Education & Research| Jul-Sep, 9(3).
Rossi, L. N., Vajani, S., Cortinovis, I., Spreafico, F., & Menegazzo, L. (2008). Analysis of the International Classification of Headache Disorders for diagnosis of migraine and tension‐type headache in children. Developmental Medicine & Child Neurology, 50(4), 305-310. https://doi.org/10.1111/j.1469-8749.2008.02041.x.
Shahrakai, M. R., Mirshekari, H., Ghanbari, A. T., Shahraki, A. R., & Shahraki, E. (2011). Prevalence of migraine among medical students in Zahedan Faculty of Medicine (Southeast of Iran). Basic and clinical Neuroscience, 2(2), 20-25.
Shepherd, A. J. (2010). Visual stimuli, light and lighting are common triggers of migraine and headache. Journal of Light & Visual Environment, 34(2), 94-100. https://doi.org/10.2150/jlve.34.94.
Smitherman, T. A., McDermott, M. J., & Buchanan, E. M. (2011). Negative impact of episodic migraine on a university population: quality of life, functional impairment, and comorbid psychiatric symptoms. Headache: The Journal of Head and Face Pain, 51(4), 581-589. https://doi.org/10.1111/j.1526-4610.2011.01857.x.
Sutherland, H. G., & Griffiths, L. R. (2017). Genetics of migraine: insights into the molecular basis of migraine disorders. Headache: The Journal of Head and Face Pain, 57(4), 537-569. https://doi.org/10.1111/head.13053.
Sutherland, H. G., Albury, C. L., & Griffiths, L. R. (2019). Advances in genetics of migraine. The journal of headache and pain, 20(1), 72. https://doi.org/10.1186/s10194-019-1017-9.
Taehtinen, R. E., Sigfusdottir, I. D., Helgason, A. R., & Kristjansson, A. L. (2014). Electronic screen use and selected somatic symptoms in 10–12 year old children. Preventive medicine, 67, 128-133. https://doi.org/10.1016/j.ypmed.2014.07.017.
Torsheim, T., Eriksson, L., Schnohr, C. W., Hansen, F., Bjarnason, T., & Välimaa, R. (2010). Screen-based activities and physical complaints among adolescents from the Nordic countries. BMC public health, 10(1), 324. https://doi.org/10.1186/1471-2458-10-324.
Vlajinac, H., Šipetić, S., Džoljić, E., Maksimović, J., Marinković, J., & Kostić, V. (2003). Some lifestyle habits of female Belgrade university students with migraine and non-migraine primary headache. The Journal of headache and pain, 4(2), 67. https://doi.org/10.1007/s10194-003-0033-x.
Vuković, V., Plavec, D., Pavelin, S., Jančuljak, D., Ivanković, M., & Demarin, V. (2010). Prevalence of migraine, probable migraine and tension-type headache in the Croatian population. Neuroepidemiology, 35(1), 59-65. https://doi.org/10.1159/000310940.
Wahab, K. W., & Ugheoke, A. J. (2009). Migraine: prevalence and associated disability among Nigerian undergraduates. Canadian journal of neurological sciences, 36(2), 216-221. https://doi.org/10.1017/s0317167100006570.
Wang, X. P., Liu, J. M., & Zhao, Y. B. (2008). Migraine: Sex-influenced trait model?. Medical hypotheses, 71(1), 14-21. https://doi.org/10.1016/j.mehy.2007.12.015.
Warhurst, S., Rofe, C. J., Brew, B. J., Bateson, D., McGeechan, K., Merki-Feld, G. S., ... & Tomlinson, S. E. (2018). Effectiveness of the progestin-only pill for migraine treatment in women: a systematic review and meta-analysis. Cephalalgia, 38(4), 754-764. https://doi.org/10.1177/0333102417710636.
Weitzel, K. W., Strickland, J. M., Smith, K. M., & Goode, J. V. (2001). Gender-specific issues in the treatment of migraine. The journal of gender-specific medicine: JGSM: the official journal of the Partnership for Women's Health at Columbia, 4(1), 64-74.
Yazdanparast, M., Abrishamizadeh, A. A., Mahboobi, H., Omrani, A., Ghasemi, M., Ghorashi, M., ... & Karimi, Z. (2013). Prevalence of and factors associated with migraine in medical students at BandarAbbas, Southern Iran, in 2012. Electronic physician, 5(3), 679. https://doi.org/10.14661/2013.679-684.
Al-Hashel, J. Y., Ahmed, S. F., Alroughani, R., & Goadsby, P. J. (2014). Migraine among medical students in Kuwait University. The journal of headache and pain, 15(1), 26, 1-6. https://doi.org/10.1186/1129-2377-15-26.
Alshammari, Y. H. M., Aldoghmi, A. K. B., AlAfif, H. S. A., Alfayi, B. A., Alrebh, A. H., Alsayafi, Z. A., Fatani, Y. A., Aldughmi, A. N., Alzaidan, A. M., Alsubaiei, S. A. O. & Alqethami, S. S. (2019). Multiple Sclerosis Diagnosis and Management: A simple Literature Review. Archives of Pharmacy Practice, 10(4), 33-37.
Amayo, E. O., Jowi, J. O., & Njeru, E. K. (2002). Headache associated disability in medical students at the Kenyatta National Hospital, Nairobi. East African medical journal, 79(10), 519-523. https://doi.org/10.4314/eamj.v79i10.8813.
Balaban, H., Semiz, M., Şentürk, İ. A., Kavakçı, Ö., Cınar, Z., Dikici, A., & Topaktaş, S. (2012). Migraine prevalence, alexithymia, and post-traumatic stress disorder among medical students in Turkey. The journal of headache and pain, 13(6), 459-467.
Bessisso, M. S., Bener, A., Elsaid, M. F., Al-Khalaf, F. A., & Huzaima, K. A. (2005). Pattern of headache in school children in the State of Qatar. Saudi medical journal, 26(4), 566-570.
Bigal, M. E., Liberman, J. N., & Lipton, R. B. (2006). Age-dependent prevalence and clinical features of migraine. Neurology, 67(2), 246-251. https://doi.org/10.1212/01.wnl.0000225186.76323.69.
Brandes, J. L. (2006). The influence of estrogen on migraine: a systematic review. Jama, 295(15), 1824-1830. https://doi.org/10.1001/jama.295.15.1824.
Deleu, D., Khan, M. A., Humaidan, H., Al Mantheri, Z., & Al Hashami, S. (2001). Prevalence and clinical characteristics of headache in medical students in Oman. Headache: The Journal of Head and Face Pain, 41(8), 798-804. https://doi.org/10.1046/j.1526-4610.2001.01146.x.
Domingues, R. B., Cezar, P. B., Schmidt Filho, J., Moraes Filho, M. N. D., Pinheiro, M. N., Marchiori, J. G., ... & Domingues, S. A. (2009). Prevalence and impact of headache and migraine among Brazilian Tupiniquim natives. Arquivos de neuro-psiquiatria, 67(2B), 413-415. https://doi.org/10.1590/S0004-282X2009000300008.
Ducros, A., Tournier-Lasserve, E., & Bousser, M. G. (2002). The genetics of migraine. The Lancet Neurology, 1(5), 285-293. https://doi.org/10.1016/S1474-4422(02)00134-5.
Ertas, M., Baykan, B., Orhan, E. K., Zarifoglu, M., Karli, N., Saip, S., ... & Siva, A. (2012). One-year prevalence and the impact of migraine and tension-type headache in Turkey: a nationwide home-based study in adults. The journal of headache and pain, 13(2), 147. https://doi.org/10.1007/s10194-011-0414-5.
Ezeala-Adikai, B. A., Ekenze, O. S., & Onwuekwe, I. O. (2013). Frequency and pattern of migraine among medical and nursing students at Enugu, South East Nigeria. The journal of headache and pain, 14(1), 1-1. https://doi.org/10.1186/1129-2377-14-s1-p5.
Ferri-de-Barros, J. E., Alencar, M. J. D., Berchielli, L. F., & Castelhano Junior, L. C. (2011). Headache among medical and psychology students. Arquivos de neuro-psiquiatria, 69(3), 502-508. https://doi.org/10.1590/s0004-282x2011000400018.
Fillingim, R. B., Hastie, B. A., Ness, T. J., Glover, T. L., Campbell, C. M., & Staud, R. (2005). Sex-related psychological predictors of baseline pain perception and analgesic responses to pentazocine. Biological psychology, 69(1), 97-112. https://doi.org/10.1016/j.biopsycho.2004.11.008.
Fountaine, C. J., Liguori, G. A., Mozumdar, A., & Schuna Jr, J. M. (2011). Physical activity and screen time sedentary behaviors in college students. International Journal of Exercise Science, 4(2), 3.
Galinović, I., Vuković, V., Trošelj, M., Antić, S., & Demarin, V. (2009). Migraine and tension-type headache in medical students: a questionnaire study. Collegium antropologicum, 33(1), 169-173.
Gasbarri, A., Arnone, B., Pompili, A., Cifariello, A., Marini, C., Tavares, M. C., & Tomaz, C. (2008). Emotional memory and migraine: Effects of amitriptyline and sex related difference. Behavioural brain research, 189(1), 220-225. https://doi.org/10.1016/j.bbr.2007.12.009.
Ghorbani, A., Abtahi, S. M., Fereidan-Esfahani, M., Abtahi, S. H., Shemshaki, H., Akbari, M., & Mehrabi-Koushki, A. (2013). Prevalence and clinical characteristics of headache among medical students, Isfahan, Iran. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, 18(Suppl 1), S24.
Gu, X., & Xie, Y. (2018). Migraine attacks among medical students in Soochow University, Southeast China: a cross-sectional study. Journal of pain research, 11, 771. https://doi.org/10.2147/JPR.S156227.
Guo, Y., Xu, S., Nie, S., Han, M., Zhang, Y., Chen, J., ... & Liu, X. (2019). Female versus male migraine: an event-related potential study of visual neurocognitive processing. The journal of headache and pain, 20(1), 38. https://doi.org/10.1186/s10194-019-0995-y.
Harle, D. E., Shepherd, A. J., & Evans, B. J. (2006). Visual stimuli are common triggers of migraine and are associated with pattern glare. Headache: The Journal of Head and Face Pain, 46(9), 1431-1440. https://doi.org/10.1111/j.1526-4610.2006.00585.x.
Houinato, D., Adoukonou, T., Ntsiba, F., Adjien, C., Avode, D. G., & Preux, P. M. (2010). Prevalence of migraine in a rural community in south Benin. Cephalalgia, 30(1), 62-67. https://doi.org/10.1111/j.1468-2982.2009.01894.x.
Iannotti, R. J., Kogan, M. D., Janssen, I., & Boyce, W. F. (2009). Patterns of adolescent physical activity, screen-based media use, and positive and negative health indicators in the US and Canada. Journal of Adolescent Health, 44(5), 493-499. https://doi.org/10.1016/j.jadohealth.2008.10.142.
Kurt, S., & Kaplan, Y. (2008). Epidemiological and clinical characteristics of headache in university students. Clinical neurology and neurosurgery, 110(1), 46-50. https://doi.org/10.1016/j.clineuro.2007.09.001.
Lampl, C., Buzath, A., Baumhackl, U., & Klingler, D. (2003). One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia, 23(4), 280-286. https://doi.org/10.1046/j.1468-2982.2003.00509.x.
Lipton, R. B., & Bigal, M. E. (2005). Migraine: epidemiology, impact, and risk factors for progression. Headache: The Journal of Head and Face Pain, 45, S3-S13. https://doi.org/10.1111/j.1526-4610.2005.4501001.x.
Liverman, C. S., Brown, J. W., Sandhir, R., McCarson, K. E., & Berman, N. E. (2009). Role of the oestrogen receptors GPR30 and ERα in peripheral sensitization: relevance to trigeminal pain disorders in women. Cephalalgia, 29(7), 729-741. https://doi.org/10.1111/j.1468-2982.2008.01789.x.
Lušić, I. (2001). Population variation in migraine prevalence–the unsolved problem. Collegium antropologicum, 25(2), 695-701.
Martín, H., Del Río, M. S., De Silanes, C. L., Álvarez‐Linera, J., Hernández, J. A., & Pareja, J. A. (2011). Photoreactivity of the occipital cortex measured by functional magnetic resonance imaging–blood oxygenation level dependent in migraine patients and healthy volunteers: pathophysiological implications. Headache: The Journal of Head and Face Pain, 51(10), 1520-1528. https://doi.org/10.1111/j.1526-4610.2011.02013.x.
Martin, V. T. (2009). Ovarian hormones and pain response: a review of clinical and basic science studies. Gender medicine, 6, 168-192. https://doi.org/10.1016/j.genm.2009.03.006.
Montagni, I., Guichard, E., Carpenet, C., Tzourio, C., & Kurth, T. (2016). Screen time exposure and reporting of headaches in young adults: A cross-sectional study. Cephalalgia, 36(11), 1020-1027. https://doi.org/10.1177/0333102415620286.
Mosarrezaii, A., & Kargar, K. (2018). Frequency of Depression in Patients with Seizure Referring to the Urmia Neuromedical Clinic and Some of the Factors Affecting it. Journal of Advanced Pharmacy Education & Research| Apr-Jun, 8, 2.
Mulder, E. J., Van Baal, C., Gaist, D., Kallela, M., Kaprio, J., Svensson, D. A., ... & Boomsma, D. I. (2003). Genetic and environmental influences on migraine: a twin study across six countries. Twin Research and Human Genetics, 6(5), 422-431. https://doi.org/10.1375/136905203770326420.
Neut, D., Fily, A., Cuvellier, J. C., & Vallée, L. (2012). The prevalence of triggers in paediatric migraine: a questionnaire study in 102 children and adolescents. The journal of headache and pain, 13(1), 61-65. https://doi.org/10.1007/s10194-011-0397-2.
Noor, T., Sajjad, A., & Asma, A. (2016). Frequency, character and predisposing factor of headache among students of medical college of Karachi. J Pak Med Assoc, 66(2), 159-164.
Polderman, T. J., Benyamin, B., De Leeuw, C. A., Sullivan, P. F., Van Bochoven, A., Visscher, P. M., & Posthuma, D. (2015). Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nature genetics, 47(7), 702. https://doi.org/10.1038/ng.3285.
Radtke, A., & Neuhauser, H. (2009). Prevalence and burden of headache and migraine in Germany. Headache: The Journal of Head and Face Pain, 49(1), 79-89. https://doi.org/10.1111/j.1526-4610.2008.01263.x.
Ramadan, M., Mohammad, B., Karim Hussein, A. N., & Ahmed, A. (2019). The effect of long term treatment with betablockers in increasing the incidence of bradycardia in patients undergoing posterior segment eye surgeries. Journal of Advanced Pharmacy Education & Research| Jul-Sep, 9(3).
Rossi, L. N., Vajani, S., Cortinovis, I., Spreafico, F., & Menegazzo, L. (2008). Analysis of the International Classification of Headache Disorders for diagnosis of migraine and tension‐type headache in children. Developmental Medicine & Child Neurology, 50(4), 305-310. https://doi.org/10.1111/j.1469-8749.2008.02041.x.
Shahrakai, M. R., Mirshekari, H., Ghanbari, A. T., Shahraki, A. R., & Shahraki, E. (2011). Prevalence of migraine among medical students in Zahedan Faculty of Medicine (Southeast of Iran). Basic and clinical Neuroscience, 2(2), 20-25.
Shepherd, A. J. (2010). Visual stimuli, light and lighting are common triggers of migraine and headache. Journal of Light & Visual Environment, 34(2), 94-100. https://doi.org/10.2150/jlve.34.94.
Smitherman, T. A., McDermott, M. J., & Buchanan, E. M. (2011). Negative impact of episodic migraine on a university population: quality of life, functional impairment, and comorbid psychiatric symptoms. Headache: The Journal of Head and Face Pain, 51(4), 581-589. https://doi.org/10.1111/j.1526-4610.2011.01857.x.
Sutherland, H. G., & Griffiths, L. R. (2017). Genetics of migraine: insights into the molecular basis of migraine disorders. Headache: The Journal of Head and Face Pain, 57(4), 537-569. https://doi.org/10.1111/head.13053.
Sutherland, H. G., Albury, C. L., & Griffiths, L. R. (2019). Advances in genetics of migraine. The journal of headache and pain, 20(1), 72. https://doi.org/10.1186/s10194-019-1017-9.
Taehtinen, R. E., Sigfusdottir, I. D., Helgason, A. R., & Kristjansson, A. L. (2014). Electronic screen use and selected somatic symptoms in 10–12 year old children. Preventive medicine, 67, 128-133. https://doi.org/10.1016/j.ypmed.2014.07.017.
Torsheim, T., Eriksson, L., Schnohr, C. W., Hansen, F., Bjarnason, T., & Välimaa, R. (2010). Screen-based activities and physical complaints among adolescents from the Nordic countries. BMC public health, 10(1), 324. https://doi.org/10.1186/1471-2458-10-324.
Vlajinac, H., Šipetić, S., Džoljić, E., Maksimović, J., Marinković, J., & Kostić, V. (2003). Some lifestyle habits of female Belgrade university students with migraine and non-migraine primary headache. The Journal of headache and pain, 4(2), 67. https://doi.org/10.1007/s10194-003-0033-x.
Vuković, V., Plavec, D., Pavelin, S., Jančuljak, D., Ivanković, M., & Demarin, V. (2010). Prevalence of migraine, probable migraine and tension-type headache in the Croatian population. Neuroepidemiology, 35(1), 59-65. https://doi.org/10.1159/000310940.
Wahab, K. W., & Ugheoke, A. J. (2009). Migraine: prevalence and associated disability among Nigerian undergraduates. Canadian journal of neurological sciences, 36(2), 216-221. https://doi.org/10.1017/s0317167100006570.
Wang, X. P., Liu, J. M., & Zhao, Y. B. (2008). Migraine: Sex-influenced trait model?. Medical hypotheses, 71(1), 14-21. https://doi.org/10.1016/j.mehy.2007.12.015.
Warhurst, S., Rofe, C. J., Brew, B. J., Bateson, D., McGeechan, K., Merki-Feld, G. S., ... & Tomlinson, S. E. (2018). Effectiveness of the progestin-only pill for migraine treatment in women: a systematic review and meta-analysis. Cephalalgia, 38(4), 754-764. https://doi.org/10.1177/0333102417710636.
Weitzel, K. W., Strickland, J. M., Smith, K. M., & Goode, J. V. (2001). Gender-specific issues in the treatment of migraine. The journal of gender-specific medicine: JGSM: the official journal of the Partnership for Women's Health at Columbia, 4(1), 64-74.
Yazdanparast, M., Abrishamizadeh, A. A., Mahboobi, H., Omrani, A., Ghasemi, M., Ghorashi, M., ... & Karimi, Z. (2013). Prevalence of and factors associated with migraine in medical students at BandarAbbas, Southern Iran, in 2012. Electronic physician, 5(3), 679. https://doi.org/10.14661/2013.679-684.